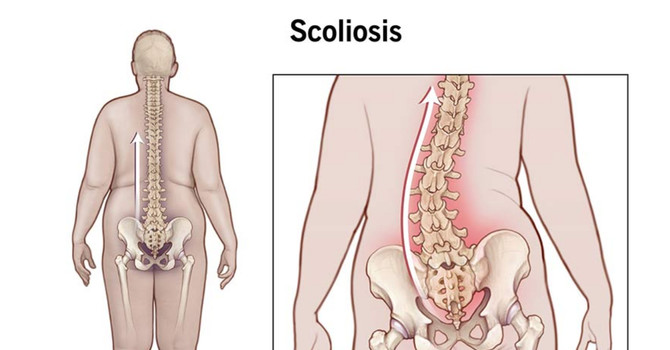
Disc herniation and pinched nerves are closely related but distinct conditions. A herniated disc occurs when the inner nucleus of an intervertebral disc pushes through a tear in its outer annulus, often due to degeneration, dehydration, injury, or uneven spinal loading. This structural change can compress nearby nerves, resulting in what is commonly referred to as a pinched nerve. However, nerve compression itself does not cause disc herniation, and pinched nerves can arise from other factors such as bulging discs, spinal stenosis, bone spurs, or spinal deformities like scoliosis.
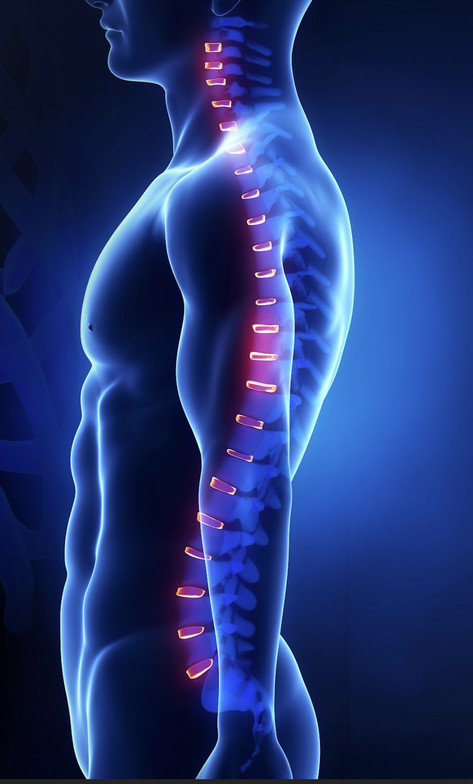
Healthy intervertebral discs are essential for spinal structure, flexibility, and shock absorption, while spinal nerves enable communication between the brain and body. When disc health deteriorates, nerve irritation, pain, weakness, numbness, or radiating symptoms can develop, with the pattern of symptoms depending on whether the cervical, thoracic, or lumbar spine is involved. For example, lumbar disc herniation may contribute to sciatic-type symptoms, while cervical involvement can affect the neck and upper extremities.
Conditions such as scoliosis increase the risk of disc degeneration and nerve compression due to abnormal spinal curvature and uneven mechanical stress. Effective management of disc herniation or pinched nerves requires identifying and addressing the underlying cause. Treatment commonly focuses on reducing mechanical pressure through condition-specific chiropractic care, physical therapy, rehabilitative exercise, lifestyle modification, and, when present, targeted scoliosis management. Addressing both disc and nerve health is essential to preserving spinal function and preventing progression or long-term nerve damage.
This topic is explored further in Pinched Nerve vs Herniated Disc: Key Symptoms & Relief clinical article published by the CLEAR Institute, which outlines how structural findings on imaging can guide diagnosis and care.

Admin
Contact Me